Illuminating the human body
Evolving from candlelight and mirrors to advanced fiber optics that provide high-performance illumination, modern tools for minimally invasive surgery enable precise, life-saving operations through natural openings or small incisions. The evolution in technology is not only why Dr. Jesse Houghton, Senior Medical Director of Gastroenterology at Southern Ohio Medical Center, can perform over a thousand minimally invasive gastrointestinal procedures annually. It is also the driving force behind broader innovations in global health, such as AI, robotic surgeries, and promising cancer treatments.
The evolution of fiber optic technology ignites innovation and advances global health.
- Modern endoscopes, which evolved from simple systems of candlelight and mirrors, now transmit high-resolution images and allow for complex procedures through natural openings or small incisions, dramatically improving patient outcomes.
- Dr. Jesse Houghton, a gastroenterologist in the US, utilizes advanced endoscopic technology to perform minimally invasive surgeries, enabling him to detect and treat gastrointestinal conditions more effectively than ever before.
- Continued innovation in fiber optic technology, including high-quality light transmission and integration with AI and robotic systems, is expanding the capabilities of minimally invasive medical procedures.
Standing on a padded mat to protect his knees, ankles, and hips from long hours in the operating room, Dr. Jesse Houghton prepares for a potentially life-saving operation on the sleeping patient in front of him. As Senior Medical Director of Gastroenterology at the Southern Ohio Medical Center in Portsmouth, Ohio, Jesse wields generational expertise and technological advancements that enable him to go where centuries of doctors never could – deep inside the human body.
“The type of scopes I use -- upper endoscope, colonoscope, duodenoscope – allow me to better detect polyps that can be hidden in the lining of the colon, for example,” Jesse says. Such an operation is one he and his practice perform over one thousand times a year, which is a testament to the skill and evolution of the technology that has allowed minimally invasive surgery to thrive.
Because for the majority of human existence, medical conditions that arose in the gastrointestinal tract – from polyps and ulcers to internal bleeding and inflammatory diseases – were extremely difficult, if not impossible, to diagnose and treat effectively. Without the ability to visualize the interior of a hollow organ or cavity in the body, treatment largely depended on external symptoms and complications like bleeding – leaving infections, diseases, or growths to go unnoticed until it was too late.
Today, the National Institutes of Health (NIH) estimates roughly 20 million gastrointestinal endoscopies are performed in the United States every year. 100 years ago, a majority of those 20 million operations, would have been considered all but impossible.
So, how did we get here?
Guided by light: Minimally invasive surgery
Historically, operations in areas of the body that were hard to access required major surgeries and massive incisions to properly illuminate the surgical field. In search of a solution, doctors, scientists, and medical pioneers spent decades searching for a way to see areas inside the human body without requiring large open surgeries.

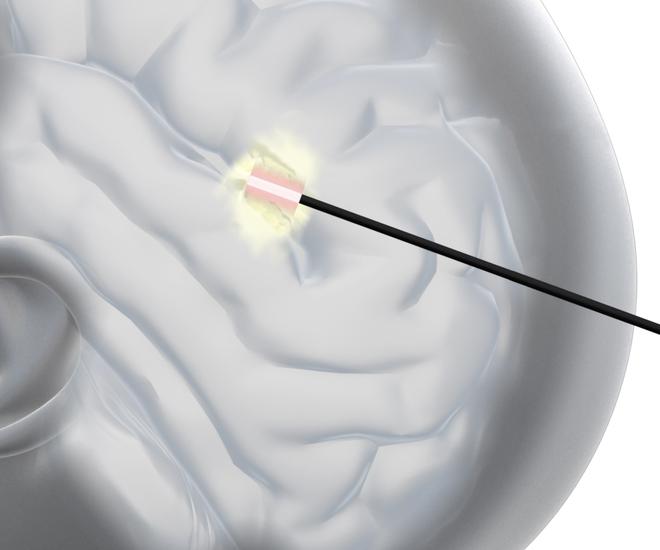
The culmination of a century of research and development is the modern endoscope. Beginning as a simple system of candlelight and mirrors invented in 1806 by German physician Philipp Bozzini, today’s endoscopes are tubular instruments that are only a few millimeters thick and can transmit high quality light inside the body, while transmitting high-resolution, real-time images back out.
Sustained endoscopic innovation has enabled doctors to see and inspect areas deep into the body by way of natural openings or very small, administered incisions. Endoscopes even allow doctors to perform life-prolonging surgical procedures, such as sampling or removing a tumor in the patient’s digestive tract.
Back in the operating room, Jesse is accompanied by a certified registered nurse anesthetist (CRNA) who monitors the vital signs of the patient while administering the sedative medication, an endoscopy technician who assists the doctor with biopsies and tools, and a registered nurse who helps monitor the patient and document times, biopsies, and medications.
"In my left hand, I operate two buttons that allow air insufflation to open the lumen of the GI tract, suctioning, and water spray to clean the lens of the scope,” he explains. “And two wheels on the scope that deflect the bottom part of the scope tube up, down, left and right.”
In the opposite hand, the doctor directs the tube of the scope inward to examine the entire area of the GI tract. “At the tip of the scope tube is a bright light, a camera lens, and a working channel where we can take biopsies and insert tools,” Jesse explains.
“The images caught by the camera lens are fed back to a processor on a shelf unit, which then feeds to an HD monitor attached to a swivel and hanging from the ceiling above the patient,” he continues. “Thanks to the endoscope's strong white light, the detailed, high-definition image is projected onto the monitor in true-to-life colors. This image is magnified several-fold, which allows me to better detect polyps that can be hidden in the lining of the colon – most of which have the potential to turn into colon cancer.”
Dr. Houghton practices full time as the Senior Medical Director of Gastroenterology at Southern Ohio Medical Center. He performs approximately 1,000 upper endoscopies and colonoscopies each, every year. He has also authored the book “What Your Doctor Doesn’t (Have the Time to) Tell You: The Gastrointestinal System”.

The efficacy of such minimally invasive surgery is perhaps best exemplified by gall bladder surgery. In the past, surgeons like Jesse would be required to cut a patient’s abdomen wide open to have enough space to adequately perform the operation. As a result, the life-saving procedure often left large visible scars, and required an extended amount of time to heal.
Today, the surgery is performed minimally invasively with a rigid endoscope – called a laparoscope when used in the abdomen – and only requires three to four small incisions in the skin for the scope and other surgical instruments such as scissors, suction devices or staplers. The abdominal cavity is filled with gas so that it expands and sufficiently allows organs to be inspected, then doctors remove the gallbladder using several instruments.
This minimally invasive option has been the preferred way to remove gallbladders since the mid-nineties. In the United States, roughly 75% of all gallbladders are removed using this minimal laparoscopic approach, while in Germany and France, that percentage is rising to 90 and above.
Fiber optic innovation with specialty glass
Since 1964, SCHOTT has expanded its material production of glass optical fibers, which are the basis of endoscopic light guides, to meet the demanding requirements of surgeons.
“While fiber optics has been around for ages, there is still so much to learn about how glass fibers can be processed, and where they can be used to improve the performance of the final devices,” explains Jan Philipp Steigleder, Senior Product Manager Medical. “And especially in medtech, where fiber-based optics are a high-performance material, it’s exciting to discover more about its physical, chemical, and mechanical versatility every day.”
Jan Philipp Steigleder is Senior Product Manager Medical at SCHOTT Lighting and Imaging. With a bachelor’s degree in Process Engineering, he joined SCHOTT in 2007 and has held various positions in R&D as well as Lighting and Imaging, most recently as Application Engineer and Senior Technical Sales Manager.

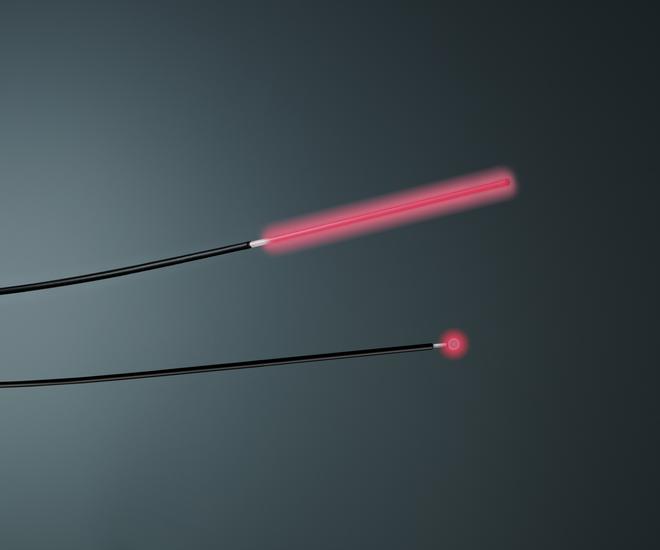
Transmitting an extremely white, neutral, and bright light that is stable over long distances, the PURAVIS® glass fibers from SCHOTT enable doctors to diagnose problems and perform surgeries more precisely.
According to Jan, this breakthrough in light transmission required a special design of glass optical fibers. "The fiber consists of two glasses with different refractive indices, the fiber core rod, and a cladding tube,” he explains. “This means the light is reflected within the fiber and transmitted to its end – these step-index fibers, therefore, ensure that the light is transmitted with as little loss as possible.”
But for its humble beginnings as a system of candles and mirrors, the endoscope remains at the forefront of medical innovation, driving improvements in patient care and outcomes. And in the same way the technology evolved from merely transmitting light to transmitting visual data – endoscopic innovation and evolution go hand in hand with the broader innovations in healthcare, such as artificial intelligence and robotic surgeries.
In other words, as new technologies emerge and evolve, so too must the endoscope.
What’s next: Robotic surgery, AI diagnostics, and beyond
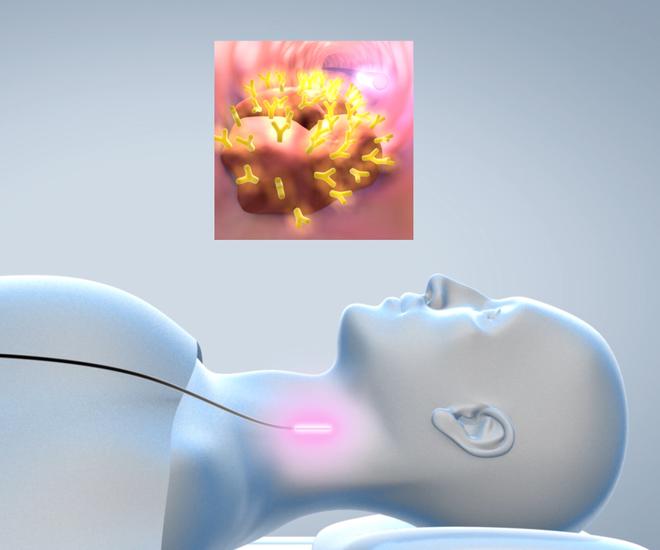
Standing at the cutting edge of such advancements are the highly specialized surgical robots that support surgeons to perform procedures. Viewing a three-dimensional image of the surgical area via cameras while sitting at a console, doctors remotely control robotic arms that compensate for any unconscious movements the surgeon's hand might make.

This brings surgical precision to an entirely new level. But even then, tightly-controlled robotic arms still rely on the operator’s ability to see inside the operating area. This means that surgeons need bright, homogeneous white light which travels several meters or around 20 feet from the light source into the body to illuminate the operating area, and transmit back images of human tissue that appear as natural as possible to the human eye.
“In technical jargon, the light needs to have a very high Color Rendering Index (CRI),” Jan explains. Lacking an adequate CRI might lead to deviations in color, which could cause doctors to overlook or misinterpret what they see inside the body, resulting in a misdiagnosis. But, when the console in front of them presents a razor-sharp image of the surgical field, doctors can perform the operation as if using their own eyes and arms.
Adapting to new technologies like surgical robotics, high-performance endoscopes have become sophisticated medical devices. “Many of the discussions and innovations in our technology center today focus on how to minimize a customer’s overall system size while increasing light output performance,” Jan explains. “This can range from finding ways to arrange our flexible fibers in smart ways to maximize light transmission by reducing interfaces and heat development. The goal is always to get as much light through the endoscope into the body as possible.”
To that end, as new technologies emerge that offer even greater potential, such as artificial intelligence (AI) and 3D imaging, these scopes must integrate light as well as advanced components such as camera chips and image sensors into a very small package.
Consider artificial intelligence, which is being researched to help monitor operations by analyzing images of organs throughout medical procedures. The AI is trained with thousands of images until it recognizes patterns that human doctors might miss. Algorithms can already use multispectral imaging to check the blood flow in organs without the need for contrast agents. Thanks to high-end endoscopes, the use of various wavelengths for lighting and imaging purposes will create the opportunity for more diagnostic applications in the future.

“Technology in endoscopes and healthcare in general continues to evolve over time,” Jesse says, noting that he’s seen a big difference since he started practicing in 2008. “Better technology that results in better image quality, paired with the most up-to-date tools available, gives me and other doctors the best chance at finding and removing things like polyps that could otherwise turn into cancer or other life-threatening conditions,” he concludes, “so even the most minor improvements have the potential to save more lives.”