mRNA: Message in a bottle for the immune system
It may sound like science fiction, but it's not: your body can produce its own vaccine and help itself fight off harmful viruses in a targeted manner – using new types of mRNA (or, "messenger RNA") vaccines. The trick is to send the blueprint for specific proteins to cells in the body via a "message in a bottle," which trains your immune system to fight unwanted invaders. If the technology has been underestimated, it won't be for long: mRNA is now one of the most promising areas of medical research, and may soon protect against cancer, malaria, and HIV.
As a key player, SCHOTT Pharma ensures safe containment and delivery of mRNA vaccines, supporting breakthroughs in medical research to combat diseases like cancer, malaria, and HIV.
- mRNA technology holds promise for personalized medicine and innovative therapies in cancer and gene therapy research.
- mRNA vaccines train the immune system to fight specific viruses.
- SCHOTT Pharma provides safe containment and delivery solutions for mRNA vaccines, ensuring that they reach patiens safely.
How the body outwits viruses with pinpoint accuracy
It's a dilemma: viruses are constantly mutating. They adapt, and more successful strains become dominant. Once reliable, vaccines can lose their effectiveness against some diseases and no longer provide adequate protection. Especially during pandemics, when many people worldwide are infected with a new virus, the long response time of traditional vaccine development and production becomes a problem.
Gene-based technologies that stimulate the body to produce its own vaccines offer new possibilities: Instead of using complete viruses and cultivating big amounts of pathogens in the laboratory or using their antigens taking plenty of time, messenger RNA vaccines send the blueprint for a protein directly into the cell. This technology enables faster production as it does not require living viruses or cell cultures. The mRNA can be synthesized directly, which speeds up the process considerably. The cell then uses the blueprint to start producing specific proteins that resemble a protein on the virus's surface. The immune system is trained to 'remember' what the proteins look like and to recognize and fight the virus once it is in the body.
Even before the pandemic, mRNA technology was researched for treating diseases other than COVID-19. Giving the body information about which proteins to make promises almost limitless possibilities in the development of drugs – and could fundamentally change medicine. This is because almost all diseases are based on faulty proteins. With mRNA, we have a kind of Swiss army knife -with the right tools for autoimmune diseases, HIV, and the treatment of tumor cells in cancer.
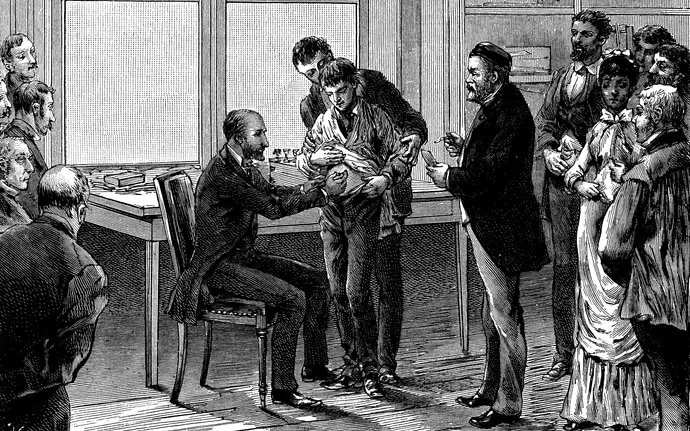
The emergence of vaccines
The search for effective protection against infectious diseases has occupied mankind for centuries. The breakthrough came in 1796 when the English doctor Edward Jenner infected a boy with cowpox, making him immune to human smallpox. There was now an effective cure for one of the most dangerous diseases in Europe.
Vaccines have continued to develop, existing ones have become more effective, and more and more people have become immune to diseases such as rabies, diphtheria, influenza, polio, and tetanus. In 1980, the World Health Organization (WHO) declared smallpox to be extinct. An unprecedented success.
How does mRNA reach its destination safely?
Telling a cell to make proteins is complicated, but sending a genetic code into cells? For a long time, this was impossible.
Consider that mRNA is instable outside cells, preventing cell-to-cell exchange. This is a mechanism against genetic miscommunication. Also in mammalian bodies, viral mRNA leads to severe inflammatory reactions - because the immune system recognizes the genetic message (just like viruses and bacteria) as foreign and fights it. This means that as long as there is no protective mechanism for the information, the messenger RNA is not suitable for conditioning the body's defenses.

This is where the research of Katalin Karikó and Drew Weissman comes in. In 2005, the two found the solution to the inflammatory reactions: Mammalian mRNA is not fought by the human body like direct information from viruses, presumably because the genetic code is slightly different. The researchers gradually modified their messenger RNA until it was no longer recognized by the immune system. They packaged the messages in liquid nanoparticles (LNPs) to do this. These lipid particles surround and protect the mRNA, like the bottle glass protecting the letter from water. This paved the way for the cell – mRNA can now theoretically be used for therapies.
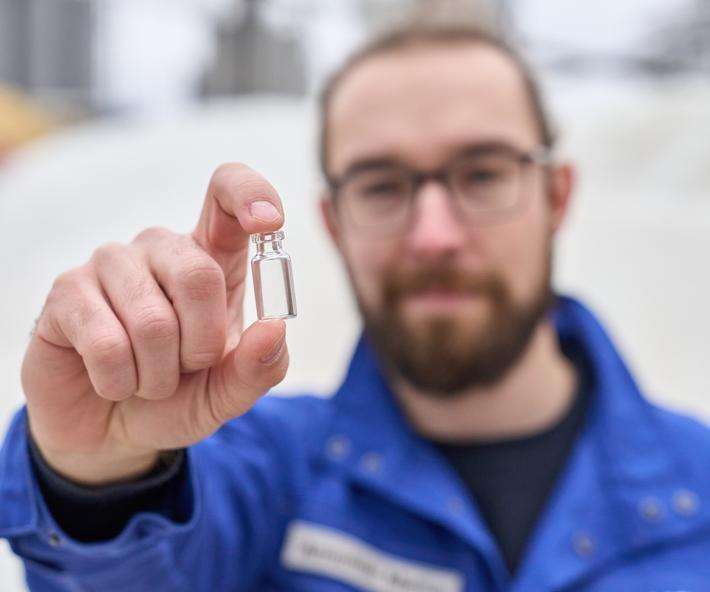
To ensure the mRNA reaches the patient in a stable state, it must be stored in suitable pharmaceutical packaging at sub-zero temperatures down to -100°C. The mRNA is usually transported in dry ice boxes to keep the temperature constant. These boxes are ideal when multiple doses of an active ingredient are packed into vials for efficient transport to vaccination centers, doctors' surgeries, and hospitals. When vaccinations are administered, the vials can be removed from the freezer and stored in standard refrigerators for several days. Given the high demand, this was an efficient system during the pandemic.
As the number of cases has declined, the need has shifted from many vaccine doses to individual doses. Future research applications are more likely to require mRNA agents in small batches -personalized medicine. This will require appropriate packaging and transport solutions.
How mRNA vaccines prepare the immune system
Despite the fact that mRNA vaccines work, several challenges must be overcome, from production to transport and storage.
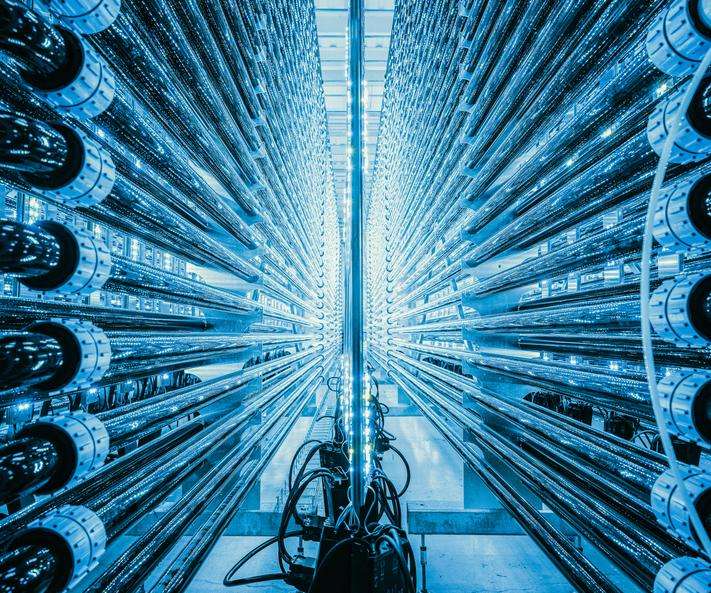
The development of an mRNA vaccine starts on the computer, where the genetic message to be introduced into the cell is defined. DNA is synthesized, and the enzyme RNA polymerase is used to produce mRNA strands. These contain important information, such as the genetic sequence for the coronavirus spike protein, which the virus uses to attach to cells.
Revolutionary research
The two researchers, biochemist Katalin Karikó and immunologist Drew Weissman, met by chance at a photocopier at the University of Pennsylvania in 1997. Karikó studied mRNA for years, first as a PhD student at the Hungarian Academy of Sciences. When she lost her job, she went to the US to continue unlocking the potential of mRNA. Weissman, on the other hand, wanted to develop a vaccine against HIV and saw the potential of Karikó's work.

Safe packaging of mRNA preparations at low temperatures
"In fact, mRNA technology only works with suitable storage solutions that can safely withstand the low temperatures which are required for the carrier material in the vaccine, the lipid nanoparticles," explains Nina Krautwurst, Global Product Manager at SCHOTT Pharma. “We develop vials as well as glass and polymer syringes in which the materials are matched to each other. With our proactive research on packaging material combinations, we supported our customers to bring their vision to life.”
Some mRNA-based vaccine or therapy approaches require extreme temperatures of -80°C and below. “Here, the polymer syringe is the solution," says Nina. “Polymer materials are less brittle than glass materials and have significantly different expansion coefficients. This can lead to cracks or fractures, for example during freezing cycles for a glass container. Tightness is also critical, as the sealing rubber stopper behaves differently to the glass itself when it freezes.”
SCHOTT Pharma is researching new solutions that can meet these demanding requirements. Syringes made of a specially developed polymer, Cyclic Olefin Copolymer (COC), are the first choice for storage at extremely low temperatures. Nina adds: "The entire syringe, including the rubber stopper on the plunger, deforms uniformly, so the drug remains securely protected. The polymer itself in combination with a cross-linked silicone layer on the inside is designed to be inert and prevent interaction with the stored drug product."
Therapies for cancer, malaria and hepatitis C
Katalin Karikó and Drew Weissman won the Nobel Prize in Medicine last year for their groundbreaking basic research into mRNA. Their discoveries have helped millions of people – and the potential to use the technology to precisely target previously untreatable diseases could change medicine forever.
The focus is no longer on SARS-CoV-2. mRNA-based therapies for bacterial infections, influenza, hepatitis C, shingles, HIV, malaria, and M-pox are also being researched. According to the German Association of Research-Based Pharmaceutical Companies (vfa), around 125 different mRNA drugs are currently in development or are already on the market.
mRNA technology also offers hope for cancer therapies that identify and destroy tumors. Cancer cells produce altered proteins because of mutations. These do not occur in healthy cells and are unique markers. This could lead to the development of personalized therapy for each cancer patient, a kind of vaccination against cancer. Companies like BioNTech and Moderna are working on several cancer vaccines in various development stages.
mRNA also holds great promise for gene therapy. Delivering a message via RNA can repair pathogenic changes in the genetic material. Initial research trials on Huntington's disease have already been successful.
The great success of mRNA vaccines has highlighted this technology's potential. It is no longer just two lone wolves who happened to meet at a photocopier and saw the potential of mRNA. Instead, technology has revolutionized and captivated an entire industry and opens a new solution spectrum to improve human health and wellbeing.