Implants for life
Paralyzed people who can move again, deaf people who can hear again, and blind people who can see again – these are not just dreams of the future; they are reality. Brain-computer interfaces (BCIs) and active medical implants (AMIs) make the previously impossible possible. Miniaturized electronics enable the brain, as well as organs and other parts of the body, to communicate with the outside world – such as computers, prostheses, or other devices – by sending information, and receiving impulses. Bi-directional communication is a key factor in modern medicine and is often the only chance for patients to improve their quality of life or even save their lives. Products and technology solutions from SCHOTT are important enablers of this medical progress.
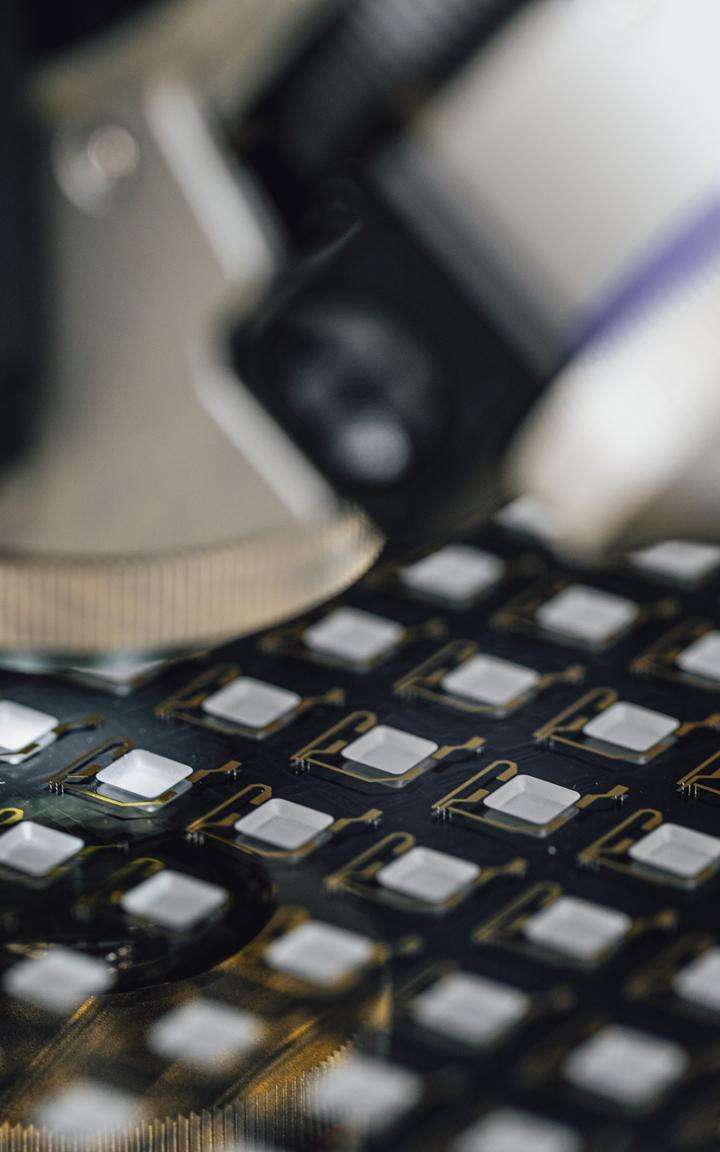
Pioneering neurotechnology: Hermetically sealed mini-implants enable patients to lead a ‘normal’ life again in the long term.
- Brain-computer interfaces (BCIs) and active medical implants (AMIs) are revolutionizing lives, e.g., enabling paralyzed individuals to move, the deaf to hear, and the blind to see.
- Medical technology has advanced since the invention of the pacemakers. Expert Claude Clement explains how and gives an insight into the fascinating potential of implants.
- SCHOTT Primoceler's glass encapsulation technology is key for next-gen medical implants, offering biocompatibility and durability. Their innovative techniques enable smaller, more efficient implants that stay safely in the body for longer.
Neurotechnology for a better quality of life
Approximately 85 billion neurons in the brain make us human. They enable complex thought processes, emotional depth, and the consciousness that distinguishes us from other creatures and controls our bodily functions. Each neuron makes 10,000 connections with other similar cells. The environment, the body, and the brain are in constant dialogue in a cosmos of electrical signals. However, this complex network is extremely vulnerable to disruption, whether due to birth defects, disease, accidents, degeneration, or age-related deterioration – with serious consequences for the health and well-being of those affected.
Since the 1960s, electronics implanted in the body have made it possible to alleviate or even eliminate neurological disorders. The focus of active medical implants (AMI) has been on the treatment of heart disease. The first patient with a pacemaker lived 43 years instead of a few months. Implantable cardiac defibrillators followed in the 1980s and 1990s.

Experience with cardiac implants laid the groundwork for neuro implants providing data on how the human body responds to long-term implantation. "The success story of medical implants began in the last millennium with the era of cardiac rhythm management," explains Claude Clement, an expert and independent consultant in active medical implants and neurotechnology. "Today, pacemakers which are connected for stimulation and sensing can be individually programmed through remote wireless communication, unlike drugs, which are made for the average person." The 21st century is the age of neurotechnology – with more complex developments such as cochlear implants for the deaf, electromechanical implants to treat severe incontinence, deep brain stimulation for Parkinson's disease, or spinal cord stimulation for pain patients.
The case of Alexis
Alexis Mayle of Louisville, Kentucky, was 22 years old when an unfortunate fall in the bathroom changed her life forever. She was diagnosed with "trigeminal neuralgia" due to their almost unbearable pain, also known as "suicide disease." After brain surgery, she was pain-free for three months - until a car hit her. The pain returned - now permanently. A neurologist diagnosed complex regional pain syndrome and offered Alexis a solution. "I had never heard of anything other than a pacemaker. But I knew I wanted the Medtronic medical implant they were proposing. It stimulates my spine to send stimuli that cause the brain to focus on sensation instead of pain."

Relief from complex symptoms
Claude also values the wide range of hands-on experiences with patients that his career has given him. One of the first was completely paralyzed from the neck down. He received a brain-computer interface in his motor cortex that reads his movement intentions and executes them by moving a cursor on the screen. Claude reports: "A first step to give mobility to a paralyzed person. Being a computer freak, he was very interested in being part of our development team.”
A young man suffering from Parkinson's disease benefited from deep brain stimulation: implanted electrodes permanently stimulate certain regions of the brain and suppress the tremors typical of Parkinson's disease by applying electricity. Claude presented the patient to his former employer, Medtronic, which was doing a lot of research in this field. The patient was ready to show who he was without stimulation, using a device that could be turned on and off. Within seconds, he was severely handicapped. "He couldn't turn the remote back on. I helped him return to his stimulated state," said Claude. "When you meet people like that, you realize the value of your work."
The engineer's engagement and passion for staying on the cutting edge of research are easily reflected in his CV. "My most exciting time was at Medtronic,” he explains. “Here, we developed sophisticated devices to treat Parkinson's disease, epilepsy, and chronic pain and tested them in preclinical studies with patient consent." His recent position at the Wyss Center in Geneva focuses on developing brain-computer interfaces. These are used to treat people with serious illnesses, such as total paralysis, by interacting between medical devices and the human nervous system. "We have advanced neurotechnology projects there to a level that is probably the highest in the world," says Claude.
A life dedicated to neurotechnology
Claude Clément (born 1955) is from French-speaking Switzerland. He began his career as head of the transducer and actuator development group in the research and development department of the Swatch Group. He entered the world of medical technology by managing Swatch's diversification activities in the field of wearable, programmable drug pumps. He then spent 27 years in the field of active implantable medical devices: as Director of Manufacturing Engineering at Intermedics (now Boston Scientific), as Operations Manager of the Swiss subsidiary of Medtronic, and later as a consultant for large companies, particularly in the field of pacemakers, and for various highly innovative start-ups. Starting in 1996, he built Medtronic's highly automated factory in the Lake Geneva region. The factory is the world's largest active implantable medical device assembly site, producing large volumes of pacemakers, defibrillators, and neurostimulators.
Until 2014, Claude was CEO of MyoPowers, a start-up company developing an electromechanical implant to treat severe incontinence. In early 2015, he joined the Wyss Center for Bio and Neuroengineering as CTO. He was the founder, chairman, or board member of several start-ups and small companies and also chairman of the BioAlps Association, a diversified life science cluster in Western Switzerland. The expert holds a master’s degree in electrical engineering from the Swiss Federal Institute of Technology (EPFL) in Lausanne and an MBA from the HEC at the University of Lausanne (Switzerland). Author of the Springer book "Brain-Computer Interface Technologies" (Springer Verlag 2019).

Experts at the Wyss Center also believe that the brain is very hostile to technological implants and that the technical barriers are very high. Over the decades, however, researchers have done pioneering work despite all the concerns. The combination of electrodes, powerful electronics, and wireless communication has made it possible to expand the interaction between the brain, nervous system, and organs and thus set new standards in neurotechnology.
BCI – brain and computer in dialog
Click on the single dots to learn more:
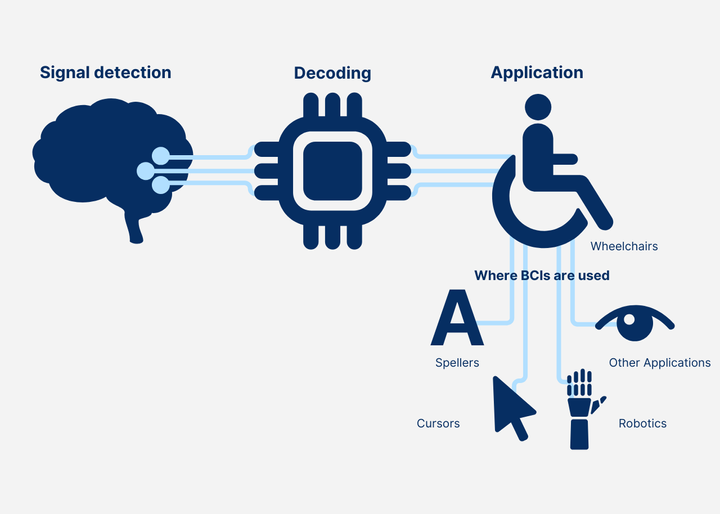


Brain-computer interfaces are revolutionizing human health. These devices can read brain activity and stimulate the brain to reactivate skills lost due to genetic predisposition, accidents, illness, or other causes.
The more data the computer receives, the better the communication results. The technology has advanced significantly: the number of individual neurons recorded simultaneously increased exponentially between 1950 and 2010, doubling every 7.4 years. Current data show an increase to 106 simultaneously recorded neurons.
AMI: What is technologically possible...
Other approved devices and treatments for nervous system disorders include:
- Programmable implantable drug pumps for chronic pain
- Gastric nerve stimulation for obesity
- Retinal implants for the blind to enable them to perceive light
- Stimulation of the tibial nerve in cases of mild urinary incontinence with external or implanted stimulation
- Functional electrical stimulation for simple movements in paralyzed patients.
Making mini-implants fit for longevity
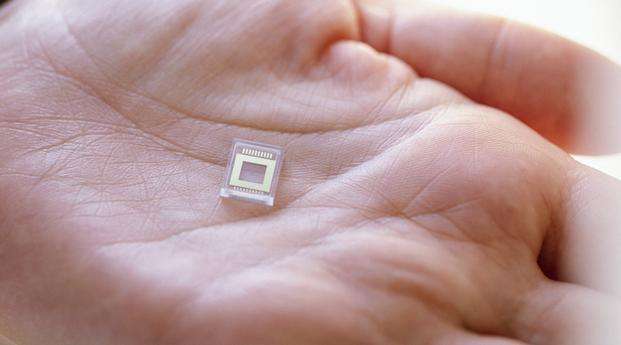
Unlike pacemakers, implants for our brain and control center must be as small as possible in order to reduce risk of the body rejecting it. In addition, the more complex their tasks, the more they need to communicate with the outside world, and vice versa. For long-term use, they must be biocompatible and stable, and there is a high risk that the body will reject the implant or encapsulate it with tissue.
"The main problem is protecting implants from moisture,” explains Claude. “And it's not easy to hermetically seal an implant. You can do it with a titanium or glass encapsulation, but you also need corresponding feedthroughs: wires that go from the inside to the outside or from the outside to the inside to carry the electrical signals.” The more channels, he continues, the more difficult it is to establish a connection to the outside world. “The key to new mini-implant technologies using high-frequency radio waves is, therefore, effective hermetic encapsulation.”
Glass: biocompatible and hermetically sealed
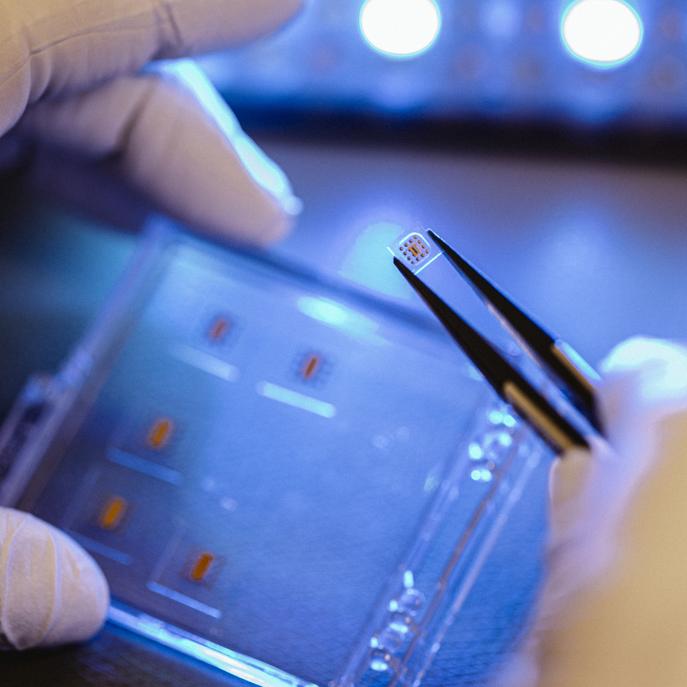
Claude found what he was looking for in one of his research projects 2018 when he contacted SCHOTT Primoceler Oy. They were looking for extremely small, biocompatible, and hermetically sealed encapsulations to build a network of tiny cells in the brain that would communicate with each other and relay information to the outside world like a mobile phone network. "Of course, they were a bit bigger than we had dreamed of,” Claude says, “but it was a first step towards a new technology".
The former startup's glass-micro bonding technology had been developed for the aerospace industry and the hermetic sealing of microelectronics in space applications. Now, it was being transferred to hermetic sealing of medical devices without fundamentally changing the processes. "So, it was a perfect fit. In my opinion, Primoceler is still the technology leader in this area of medical device encapsulation," Claude told Ville Hevonkorpi, Vice President of SCHOTT Primoceler Oy, during a visit to Tampere in Finland.
Ville: "With our laser-based glass micro-bonding, we enable completely hermetic seals for ultra-miniaturized implants, even smaller than 1 mm." The transparent, MRI-compatible glass encapsulation virtually eliminates the need for wired feedthroughs, as radio frequencies pass through the all-glass housing. This reduces the complexity and size of the components and allows them to be connected wirelessly via the internet in the future.
"Our laser processing takes place at room temperature, which opens up new possibilities for encapsulation electronics,” explains SCHOTT Primoceler Oy production manager Ossi Lahtinen. “The hermetic fusion is achieved without any additives or adhesives and solely utilizing a precise laser that bonds the different glass layers only at the contact surfaces, i.e. only a few millimeters.”
As a biocompatible material, glass can remain in the body for a long time. This is an opportunity to move away from titanium, which is difficult to miniaturize. Plus, because glass can be produced in a batch process, switching to glass encapsulation enables large batch sizes of devices to be produced cost-effectively. Thanks to standardized and highly automated processes, the quality of the products remains consistently high.
According to Claude, this “could open the door to an expanded use of implants for applications in the brain."
Miniaturized glass encapsulation enables a new level of implants
SCHOTT Primoceler’s laser-based bonding at room temperature is a groundbreaking addition to SCHOTT's portfolio of hermetic packaging technologies. Together with customers, customized solutions for demanding applications, including in the field of medical technology, are being developed.
- Hermetically sealed
- Miniaturized and compact design
- No adhesives or additives
- No ambient heat
- Biocompatible
- High yield and reproducibility
Many questions are still unanswered
Despite progress in miniaturization and promising ideas, moving neurotechnology from the laboratory to clinical practice is difficult, mainly because of unclear and risky funding. Against this background, Claude's vision for implants is cautious.
"The miniaturization of electronics is ongoing, but we still have no answers to how to power devices without batteries,” he says, “or how to add more functions without having a solution for how devices can be powered without batteries. Or how to add more functions without having a solution for the electrical feedthroughs, the encapsulation, the type of cable and the connector.”
Claude suggests a less ambitious approach. “We should use the new technology for simple devices before we fail with too complex ones,” he explains. “We should take a helicopter perspective and really understand where we are making progress at the system level."
Today, pacemakers are implanted somewhere in the world every 15 seconds. In this way, he hopes that one day it will be possible to achieve the level of implantability of a pacemaker. The new technology is still a long way from achieving its goal. "Future successes in BCIs will be determined by mastering encapsulation, connectivity, and wireless communication," Claude explains.
Pushing back against the highly-publicized vision of companies like Neuralink to connect AI and machines to healthy people to enhance their abilities, Claude argues that those who need it most should be the focus of the technology's innovation going forward. “Shouldn’t we try to help people in need, first?” he asks.
Certainly, the words of the young patient Alexis would support his statement. "The implant gave me my life back. The pain itself and the path to "freedom from pain" have made me a completely different person. I am more compassionate and empathetic; I really appreciate life the way as it should be".